Prior Authorization: The Hidden Cost of Inefficiency in Healthcare and a Smarter Way Forward
Prior Authorization: The Hidden Cost of Inefficiency in Healthcare and a Smarter Way Forward

Prior authorization (PA) was meant to control costs and ensure patients receive medically necessary care. Instead, it has become a roadblock—delaying treatment, increasing administrative work, and exhausting both providers and patients.
The numbers paint a frustrating picture:
- 14+ hours per week—that’s how much time physicians lose to PA requests. That’s nearly two full workdays.
- 24% of doctors say PA-related delays have led to serious adverse events for patients.
- 15–20% of requests are denied upfront, yet 75% of those appeals are eventually overturned—a massive waste of time and resources.
- Outdated, fragmented systems make the process even more painful—only 26% of providers have fully electronic workflows, while most are stuck using phone calls and faxes.
It’s not just an inconvenience—it’s a healthcare crisis. Delays in approvals for essential treatments like cancer therapy or heart medications can make the difference between recovery and decline. Providers are drowning in paperwork, patients are suffering, and the system is at a breaking point.
A Smarter Way Forward with AI
The future of prior authorization is here, and it’s powered by AI. CloudAstra’s AI Agents are tackling inefficiencies head-on, helping providers regain time, reduce stress, and improve patient outcomes. Here’s how:
1. AI Agents Take Over the Busywork
CloudAstra’s AI-powered assistants handle data collection, documentation verification, and request submission—eliminating manual errors and cutting down on unnecessary delays. Instead of wrestling with paperwork, providers can focus on what they do best: patient care.
2. Smarter, Faster Prior Authorization Requests
AI seamlessly integrates with EHR systems to auto-populate and submit PA requests, reducing the likelihood of denials due to missing or incorrect information. Instead of deciphering complex insurer requirements, providers get AI-driven accuracy that ensures compliance upfront.
3. AI Knows What Will Get Approved
By analyzing historical data and payer policies, CloudAstra’s AI Agents predict approval likelihood and offer proactive recommendations to improve documentation before submission. Fewer errors, fewer denials, and a much smoother process overall.
4. Automated Appeals That Actually Work
When a PA request is denied, CloudAstra’s AI immediately analyzes the reason, retrieves missing documentation, and optimizes the resubmission. No more endless back-and-forths—just faster resolutions and minimized revenue loss.
5. Less Paperwork, Less Burnout
Administrative overload is one of the biggest contributors to burnout in healthcare. By taking on repetitive tasks, AI gives providers back 10+ hours per week, freeing up time for what really matters—delivering quality care to patients.
6. Security and Compliance, Built-In
With HIPAA-compliant encryption, audit trails, and role-based access, CloudAstra AI ensures sensitive data remains secure. Standardized AI-driven workflows also help providers stay compliant with evolving regulations, eliminating guesswork and risk.
AI’s Impact on Prior Authorization Efficiency
A comparison of traditional PA versus AI-driven PA illustrates the transformative impact of automation in healthcare:
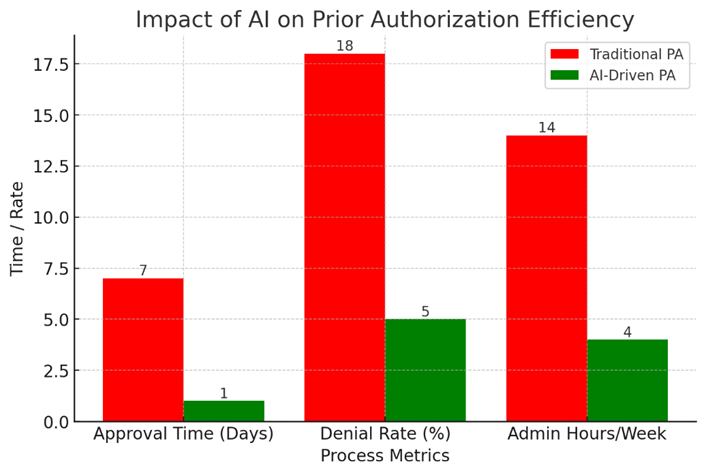
- Approval Time: Reduced from 7 days to 1 day with AI.
- Denial Rate: Dropped from 18% to 5% due to AI’s predictive documentation.
- Administrative Burden: Cut from 14 hours to 4 hours per week per provider.
The industry is Embracing AI for Prior Authorization
The momentum behind AI-driven PA is undeniable. Major healthcare organizations and insurers are making bold investments to streamline workflows and improve efficiency:
- Cigna has committed $150 million toward modernizing claims processing and patient advocacy.
- Legislators are pushing for reforms to cut through administrative red tape and accelerate approvals.
- AI-powered solutions like PAULA by Thoughtful AI are proving that prior authorization doesn’t have to be a bottleneck—it can be seamless, fast, and accurate.
As the industry moves toward automation, CloudAstra AI Agents are leading the charge. By eliminating inefficiencies, reducing costs, and improving patient care, they offer a smarter way forward for hospitals and clinics ready to embrace the future of healthcare.
The Future is Here—Are You Ready?
The traditional PA process is broken. AI-powered solutions like CloudAstra AI Agents are paving the way for a faster, smarter, and more efficient healthcare system. By automating approvals, reducing denials, and ensuring compliance, CloudAstra is setting a new standard for patient care.
The question isn’t if AI will change prior authorization—it’s when.
Ready to transform your hospital’s PA process? Let’s talk.
Contact Us:
Let us innovate together. If you are interested in exploring this further contact us at https://cloudastra.ai/contact-us