Wake Up to the Rural Health Trainwreck
WAKE UP TO THE RURAL HEALTH TRAINWRECK
The underserved healthcare market is in a crisis mode and many people have not realized the gravity of the situation. If the trend continues, it will become a full-blown crisis and fixing the broken system will be almost impossible. The unfortunate reality is that the underserved market caters to the needs of the individuals and families that need care the most. The examples of the underserved market are rural health, mental health, geriatric care etc. In this blog we will dive a little deeper into the rural health issues, what the primary causes of the problem are, and a potential solution.
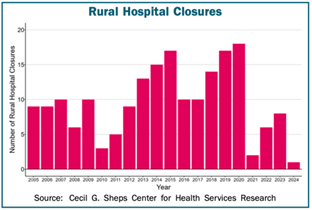
According to the Center for Healthcare Quality and Payment Reform (CHQPR), there were around 2,400 rural hospitals in 2005. Over the last 20 years, 192 of them have shut down, which is 8% of the total. Of the remaining 2,200+ hospitals1, more than half are operating at a loss, with many at risk of closing2. The following graph illustrates the seriousness of the current state:
Source: Data from CHQPR, Apr 2024

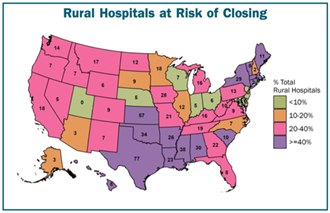
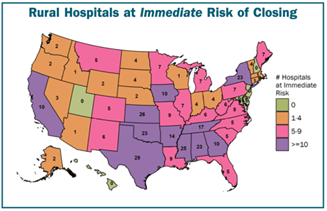
The following graphs from CHQPR shows that the problem is spread across the country and the alarming closure rate:
There are 2 primary drivers for this issue:
- Operational inefficiencies
- Low financial reserves
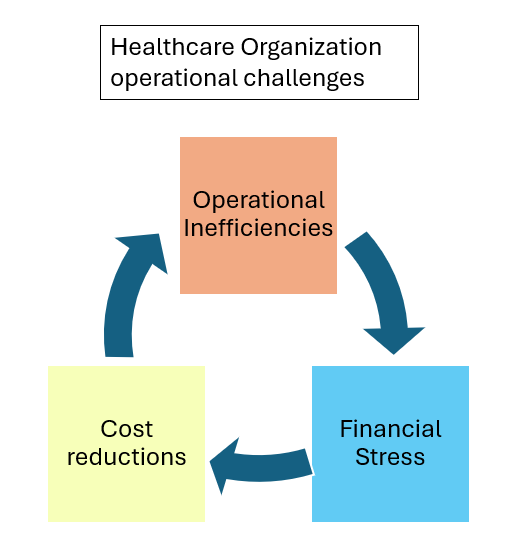
For many rural healthcare organizations, the payment for member care is through private payers, Medicare, Medicaid, and charity. The largest loss happens because private payers pay less than the cost of care delivery. The most common reason is because the healthcare organization does not have the resources or time to diligently navigate the complex processes required by the payers. There are inefficiencies in every step of the care journey, from prior authorization, patient journey, scheduling all the way through revenue cycle management. This vicious cycle of “operational inefficiencies leading to financial stress triggering further cost reductions, resulting in even more operational inefficiencies” is only creating a trainwreck in slow motion and it is time to wake up.
Worsening Challenges in Rural Healthcare Access:
Here are some of the scenarios of operational challenges faced by rural healthcare organizations and the impact to the members who need care:
- Home Health Services: The scarcity of home health agencies in rural areas has intensified, leading to more severe reimbursement issues and workforce shortages, further hindering essential home care services1.
- Hospice and Palliative Care: Workforce shortages, reimbursement issues, and limited broadband access make it increasingly difficult for rural residents to access end-of-life care, leaving many without the critical support they need during their final stages of life3.
- Mental Health Services: Access to mental health providers in rural areas has diminished, forcing residents to rely on overburdened primary care providers. Inadequate reimbursement and increased time constraints add to the difficulties in accessing mental healthcare3.

- Substance Use Disorder Services: The lack of adequate treatment services in rural communities has become more acute, making it harder for residents to access detoxification services and medication for opioid use disorder, perpetuating the cycle of addiction2.
- Reproductive, Obstetric, and Maternal Health Services: Hospital closures and limited provider availability have worsened, contributing to growing disparities in maternal and infant health outcomes3,2.
- Impact of Healthcare Facility Closures: The closure of rural healthcare facilities has accelerated, significantly impacting access to care. This trend leads to unstable health services, rising emergency medical service costs, and greater barriers to access, especially for vulnerable populations1.
Remedial Approach:
CloudAstra has built a platform that leverages the latest technological advancements to significantly reduce the operational cost of healthcare organizations. Some of the key areas where CloudAstra can help are:
- Prior Authorization Management: CloudAstra’s prior authorization management solutions streamline the approval process for medical treatments and medications. By automating and expediting prior authorization requests, rural healthcare providers can reduce delays in care delivery and improve patient outcomes, even as challenges worsen.
- Patient Flow Optimization: CloudAstra’s patient flow optimization tools enhance the efficiency of patient movement through healthcare facilities. By using AI-driven algorithms to predict patient needs and optimize scheduling, rural hospitals can reduce wait times, increase patient throughput, and ensure timely access to care amidst growing pressures.
- Revenue Cycle Management: CloudAstra’s revenue cycle management solutions streamline billing processes and optimize reimbursement, helping rural healthcare providers maximize revenue and financial sustainability. By improving revenue capture and reducing administrative burdens, organizations can reinvest resources into patient care initiatives, addressing the worsening financial constraints.
Conclusion
The challenges facing rural healthcare access have worsened significantly, making it even more critical to find effective solutions. CloudAstra’s innovative offerings provide a pathway to overcoming these escalating barriers by leveraging technology, optimizing patient flow, streamlining prior authorization, and enhancing revenue cycle processes. CloudAstra has priced itself as a low-cost barrier to entry where customers can get in for less than the cost of a cup of coffee a day per user. Together, we can bridge the widening gap in rural healthcare access and ensure that all communities have access to quality care, regardless of location or resources.
CloudAstra: we are bringing care back into healthcare.
Contact Us:
Let us innovate together. If you are interested in exploring this further contact us at https://cloudastra.ai/contact-us