Orchestrate Healthcare Revenue Cycle Management with ChatGPT – Part 2
Orchestrate Healthcare Revenue Cycle Management with ChatGPT – Part 2

This is the second in our series of blogs on Orchestrating Healthcare Revenue Cycle Management and will talk about using ChatGPT for Prior Authorization. You can find the first blog that addresses setting pricing here https://cloudastra.ai/2023/03/15/orchestrate-healthcare-revenue-cycle-management-with-chatgpt-and-robotic-process-automation-part-1-set-pricing/
What happens in Prior Authorization
When patients present themselves either via phone or in person the hospital system needs to obtain prior authorization from the payer(s) for the patient care. This step is essential to verify that the payer and provider agree together that a healthcare service, treatment plan, prescription drugs, or durable medical equipment is medically necessary and warranted. The payer would also be interested in the amount of coverage that can be preapproved for the items being preauthorized.
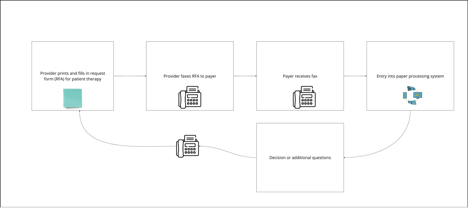
How does this happen now?
A lot of hospital systems have manual systems for the prior authorization process. This could involve manual phone calls, and emails or in some cases could involve sending information to payers using postal mail. Yes, the use of snail mail may indeed be surprising to anyone hearing it but it could be the only way some providers may be able to transmit HIPAA information in a compliant manner. Regardless of the mode of communication, there is a lot of manual effort to communicate the line items being requested and get approval.
Why does the process need to be manual?
A lot of hospital systems are not equipped with the systems to handle this communication digitally. The presence of HIPAA information complicates the exchange of information and the prior authorization workflow involves possibly complicated exchange of information such as patient history and other factors.
What is the problem with a manual system
Time consumed
There are several issues with manual systems. The first is the time that is spent on each of the transactions. Each prior authorization process could take anywhere between 5 minutes to an hour. A study by CAQH (https://www.caqh.org/insights/caqh-index-report) points to several interesting and compelling statistics.
Prior authorization transactions take a significant amount of time for healthcare providers and a fully automated solution could save 14 minutes for Medical and 10 minutes for Dental practices per transaction. This could represent a potential saving of $13.5 Billion in Cost Savings Opportunity Annually for the Medical and Dental Industries Combined Medical Industry: $12.8B Dental Industry: $664M
Patient out of the loop
Patients are typically not involved doing the prior authorization process. This leads to lower engagement on behalf of the patients and lower patient satisfaction costs.
Why fix this ?
It is economical and will save money
Fixing the manual prior authorization process will save money. As we have seen from the CAHQ study there is tremendous potential to save time and money by automating the prior authorization process.
Reduce staff burden
The automation of the prior authorization process will reduce the burden on hospital staff
Improve payments
Once the prior authorization is captured digitally it improves the payment process since there are guard rails for the submission and payment of the claim.
It is going to be legislated
The prior authorization process will soon fall under the purview of the legislation. Although this has been tried before and has not yet been implemented, the third time may be the charm and the current target date for this is Jan 2026.
Patient Satisfaction
Including the patient in the conversation is always helpful to patient satisfaction and will reduce surprises for the patient
The after/automated process
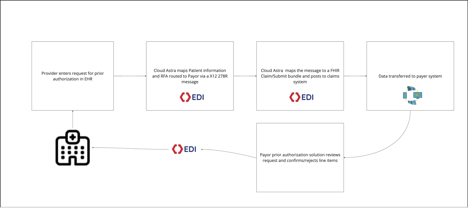
How can AI/ChatGPT and generate AI products help
Transforming the communication to EDI X12 will not necessarily solve the prior authorization puzzle. The solution has multiple components.
The first component is a machine-learning model that can learn from prior submissions and payments/denials. This model will analyze what combination of line items for example has a higher chance of denial or a chance for additional questions or queries. The model can also determine how information can be proactively sent to the payers in some cases to avoid the rounds of submission and queries.
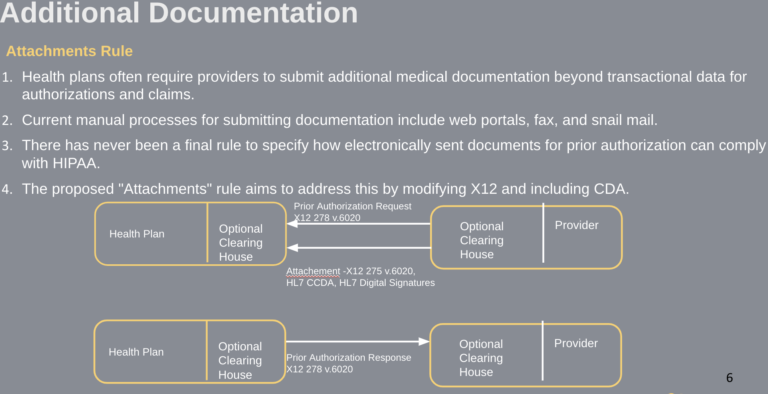
The second component is the transfer of information safely using secure EDI x12 toolsets. This addresses concerns about HIPAA and other security issues during the communication process.
The third is the translation of the requirements for prior approval from human terms to EDI. This is where chatGPT and generative AI tools come in. With the help of generative AI tools, EDI transactions can be converted to human-readable format and vice versa.
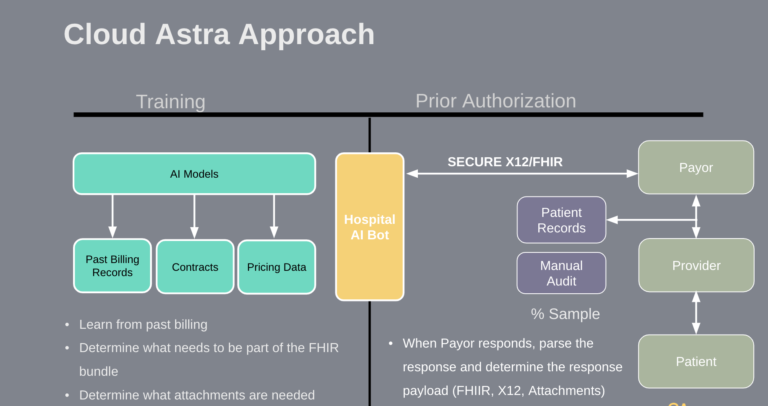
As we can see the solution to the prior authorization is a combination of utilizing past data, using machine learning to derive patterns from the data, and using generative AI to streamline the communication between systems.
At CloudAstra we are excited to use these toolsets to create savings for our client provider systems and are committed to using technology to improve healthcare workflows.
Contact Us
Let us innovate together. If you are interested in exploring this further contact us at https://cloudastra.ai/contact-us