Orchestrating Nurse Scheduling with AI and ChatGPT

What is Nurse scheduling?
Hospital systems need to schedule nurses for various departments such as ER, OR, and Inpatient. Each of these departments has slightly different methodologies in the way nurses are selected and assigned for duties. However, from an overall point of view, nurse scheduling for these areas does follow a lot of patterns and similarities.
How does nurse scheduling get set up?
The first step in nurse scheduling is a prediction of nurse requirements. Let us consider each of the departments.
In ER, nurse scheduling is largely dependent on ER census prediction. Several states have recommended nurse-to-patient ratios so that adequate care can be provided. ER census predictions can be performed using forecasting tools and using various attributes such as the day of the week, month, season, flu patterns, holiday patterns, and other such criteria. Usually, a large amount of past data is analyzed to detect the patterns and then used to forecast the census in the near term.
In, OR, the nurse scheduling is based on the prediction of the requirements for OR procedures and associated tasks. OR block schedules determine the general OR requirements during and after prime time. However, OR blocks are not completely utilized so prediction of usage patterns is needed on top of the base schedule to determine the OR utilization. Based on this, nurse requirements can be predicted in the near term.
Inpatient census is typically a combination of the ER and OR load and scheduled admission. For example, typically, 30% of ER patients could end up getting admitted. So, ER census gives a good inkling of the demand for nurses on the inpatient side.
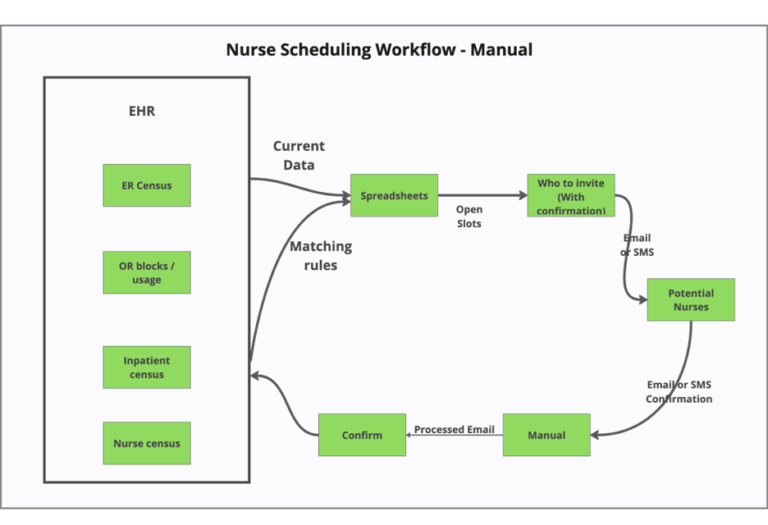
What happens currently?
Some of the nurses are on the hospital staff and some nurses are on contract and could be traveling nurses. Determining the nurse requirements and coordinating the hiring and confirmation of nurses is a largely manual process unless specific nurse management systems that deal with end-to-end nurse schedule management systems have been set up. Even if the nurse HR systems can handle nurses clocking in and out, they may still have gaps in the way nurses need to be contacted and hired for contract and peak-in jobs.
What is the problem with a manual system?
Time consumed
Manual configuration of the nurse schedules and coordinating nurse signups are messy processes that involve a lot of Email and SMS messages.
Hospital managers out of the loop
Since nurse hiring for contract jobs is a manual process, it is not easy for hospital departmental managers to stay in the loop. There may be availability and surplus on the ER side but the OR managers would not know of the surplus unless they pick up the phone and talk to other departments.
Frustrating for nurses
Answering Emails and SMS messages and waiting for replies can be frustrating for the nurses as well.
Why fix this
It is economical and will save money
Fixing the manual process for nurse scheduling will help in freeing up hospital management. Optimizing nurse blocks could also help save FTEs since the analysis of past blocks and experimenting with the block time can yield insights such as how a 9-hour block vs an 11-hour block can affect the total FTEs that are needed.
Reduce staff idle time
The automation of the nurse scheduling process can improve the staff idle time. Contrary to expectations, staff idle time is perceived negatively by the nurses as well.
Matching nurses based on qualification
Nursing spots often require nurses with specific skills and these qualifications and specializations can be added as qualification mechanisms for the automation routine.
Improve revenue
Nurses are at the heart of the medical activities and their cost comprises approximately 25% of the total hospital operating budget and 44% of the direct care costs1.
Patients at hospitals with ICU nurse–patient ratios of 1 to 3 or higher had more complications and 14% higher costs ($1,248 per patient) than those at hospitals with lower ICU nurse–patient ratios. Since the additional nursing staff increases the operating cost, an optimized and adaptive scheduling system can result in better utilization of the existing RN staff and reduce complications and costs2.
More than 3 million registered nurses (RNs) are employed in nursing (56% in hospitals), making registered nursing the largest healthcare profession. The average salary is USD 83K and the median is USD 78K, nationwide.
As per an earlier research paper, Annual medical savings per RN include $7400 from preventing nursing-sensitive adverse events (91% of which are reduced hospital costs and 9% are reduced costs for professional services and other post-discharge costs); and $38,100 for hospital-related savings and $2500 for professional services savings related to reduced LOS unassociated with preventing adverse events. Productivity benefits to society per additional FTE RN include $10,300 for reduced patient mortality and $1800 for a faster recovery3.
Improve the quality of patient care
Evidence across numerous studies has shown that the risk of mortality in a hospital setting was 9% lower in ICUs, 6% lower in medical patients, lesser by 16% for surgical patients with an additional Resident Nurse (RN) per patient day4.
Patient Satisfaction
Improved nurse scheduling will help with improved patient satisfaction.
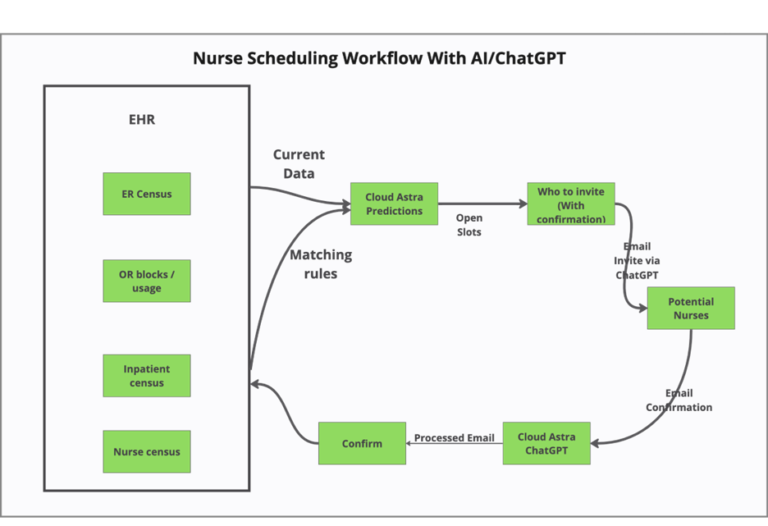
How can AI and in particular Generative AI products help?
Although several traditional nurse scheduling solutions exist in the market the advent of Generative AI could be a game changer. Imagine if hospital managers can interact with a trained bot that can answer questions like
- What is my census for the next 7 days?
- How many nurses do I need in addition to full-time staff?
- Can you email the nurses available?
- Have any nurses applied for the blocks?
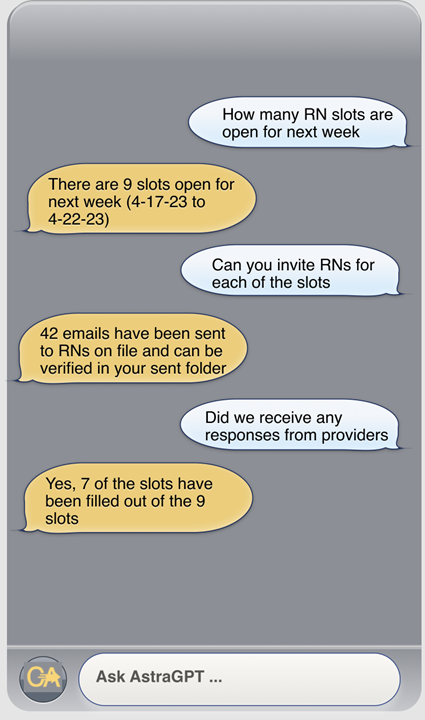
The use of generative AI will be transformative in different areas of the healthcare system, but logistical coordination activities such as Block Scheduling and Nurse Scheduling that involve a lot of spreadsheets, emails and manual activities are an ideal place to start.
Contact Us
Let us innovate together. If you are interested in exploring this further contact us at https://cloudastra.ai/contact-us
References
- Welton JM, Fisher MH, DeGrace S, Zone-Smith L (2006) Hospital nursing costs, billing, and reimbursement. Nursing Economics 24:239–45
- https://massnurses.org/files/file/Legislation-and-Politics/3_08CE_NurseStaff.pdf
- https://journals.lww.com/lww-medicalcare/Fulltext/2009/01000/The_Economic_Value_of_Professional_Nursing.14.aspx
- Nurse staffing and quality of patient care. Kane RL, Shamliyan T, Mueller C, Duval S, Wilt TJ.Evid Rep Technol Assess (Full Rep). 2007 Mar;(151):1-115.